As World Heart Day 2023 draws near, it provides an opportunity to delve into the challenges and intricacies of cardiovascular disease (CVD) in the Asia Pacific (APAC) region. In 2019, Asia recorded 58% of the 18.6 million CVD deaths worldwide. CVD claimed 10.8 million lives, which accounted for 35% of all Asian fatalities that year. Worryingly, 39% of these deaths affected individuals below 70. [1]
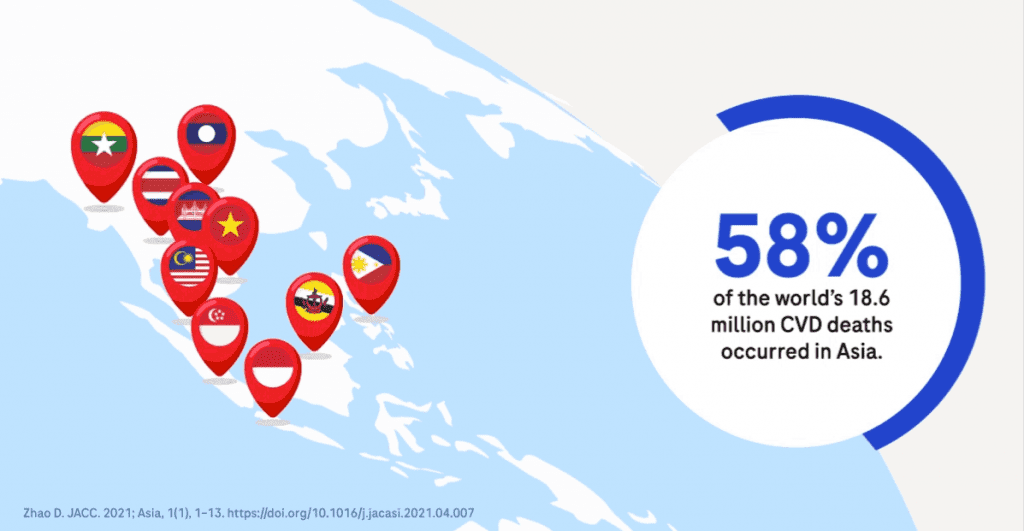
The rise in CVD can be traced back to an uptick in modifiable risk factors prevalent across most Asian nations. These include unhealthy eating habits, smoking, obesity, high blood pressure, elevated cholesterol, and diabetes. Compounding this challenge is the demographic shift with a rapidly ageing population. As of 2019, 4.8% of Asia’s populace was above 65 years old, anticipated to rise to 8.8% in 2020 and a staggering 17.8% by 2050.[2]
Despite established management guidelines, there’s a noticeable disparity in implementing recommended diagnostic procedures. The APSC APAC Consensus Statements on Chronic HF’s Diagnosis and Management underscore the importance of measures like checking natriuretic peptide levels (with a preference for NT-proBNP), undergoing TTE, and supplementary tests such as chest x-rays and electrocardiograms for suspected HF patients.[2]
However, a review of on-ground practices paints a troubling picture. For instance, an analysis of patients who succumbed to AHF in hospitals unveiled that while natriuretic peptides were accessible in over 80% of cases, only 17.9% of newly identified patients underwent testing. More alarmingly, this figure dropped to just 8.5% in the Emergency Department. This lack of clarity in diagnosis led to extended triage times and patients receiving multiple non-HF-related tests and treatments, some of which might have contributed to adverse outcomes.[3]
A mere 8.5% of patients in the Asia Pacific were given the NT-proBNP test upon hospitalisation for acute decompensated HF. This underutilisation of pivotal diagnostic tools hints at an untapped potential to enhance the region’s patient care and quality of life.[4]
There’s a clear avenue to elevate cardiovascular disease (CVD) management in the Asia Pacific region by emphasising the role of cardiac biomarkers. Fostering greater awareness and access to these crucial tests could unlock a transformative era in CVD management, with biomarkers as the key to myriad opportunities.
Empowering Heart Failure Patient Management with NT-proBNP
Utilising NT-proBNP testing alongside clinical evaluations significantly reinforces the triaging process, directing patients to appropriate care and augmenting clinical assurance.
NT-proBNP stands out as a reliable biomarker in gauging the severity of heart failure, paving the way for more informed treatment decisions. Additionally, it aids in monitoring disease progression and triaging patients who might require advanced diagnostic procedures, such as echocardiography. Furthermore, for patients with type 2 diabetes, NT-proBNP facilitates risk stratification of CVD, categorising them into high-risk and low-risk groups.
a. Demonstrating NT-proBNP Utility in Practice
Recent insights from the STRONG-HF trial, an integral part of the ESC guidelines update for HF 2023, emphasise a novel approach to acute heart failure management after hospital admission. This involves the optimisation of Guideline-Directed Medical Therapy (GDMT), which commences and adjusts oral HF medications within two weeks of the hospital discharge, followed by consistent monitoring of clinical and laboratory parameters and further up-titration to 100% of the recommended dose in the weeks immediately after discharge.[5] The STRONG-HF treatment strategy also emphasises the importance of assessing NT-proBNP biomarker levels. This approach reported a 34% relative risk reduction, translating to an 8.1% absolute risk reduction in the combined outcomes of death or heart failure readmission. Notably, there was a 26% decrease in cardiovascular deaths, a 44% reduction in heart failure readmission rates, and a 16% decline in all-cause mortality. For these excellent results, the NNT was only 12.[6]
The updated ESC guidelines advocate a vigilant observation of several health indicators during follow-up monitoring, including signs of fluid build-up, blood pressure and heart rhythm variations, NT-proBNP levels, potassium measures, serum creatinine and the estimated kidney filtration rate in follow-up visits.
However, despite the guidelines, delayed HF diagnosis and treatment are significant issues in Australia. In India, only 25% of patients were under guideline-directed medical treatment (GDMT). Studies show that, tragically, over five years, 59% of these registered patients do not survive.
This highlights the need to start GDMT right after an Acute Decompensated Heart Failure episode. Personalised treatments using point-of-care biomarkers are essential for accurate diagnosis, prognosis and digitally remote monitoring of patients.
b. Navigating HF Risk in T2DM Patients: Being in the Driver’s Seat with Cardiac Biomarkers!
Recently, type 2 diabetes (T2D) cases have surged, especially in developing countries, with Asia accounting for 60% of global diabetes cases. T2D doubles the risk of cardiovascular diseases (CVD). The intersection of T2D and heart failure presents unique challenges. The primary contributors to CVD-related deaths among T2D patients are poor blood sugar control and fluctuating glucose levels. While managing blood sugar is vital, protecting vital organs is also crucial.[7]
Diabetic patients often exhibit diastolic dysfunction, which can be traced to blood sugar irregularities and insulin issues. Undetected diastolic heart failure can emphasise the need to diagnose early diabetics. Managing diabetes and tackling obesity can reduce heart failure and overall cardiovascular deaths.
Detecting early-stage HF is challenging in T2D patients, even when multiple risk factors are present, as it often presents without symptoms.
Biomarkers like NT-proBNP play a pivotal role in early heart failure detection and provide an objective diagnostic method, acting as a “universal language” to healthcare physicians from different specialities. Particularly in T2D patients, these cardiac biomarkers are essential for stratifying HF risk. It underscores the importance of a collaborative approach where endocrinologists and cardiologists holistically manage glycemic levels and cardiac risks.
The Hong Kong Patient Support Program (PSP), as part of their assessments for complications in diabetes patients, performs NT-proBNP tests. Values above 125pg/mL indicate a heightened cardiac risk, necessitating enhanced cardiac investigations, monitoring and treatment. Japan’s Diabetes and Circulation Societies advise measuring NT-proBNP at least on an annual to 6 monthly basis, along with chest X-rays and electrocardiography for heart failure detection in at-risk diabetic patients.
The 2022 ADA Consensus recommends using cardiac biomarkers like NT-proBNP, BNP, and high-sensitive cardiac troponin for screening and diagnosing heart failure in pre-diabetic and diabetic patients. If levels are elevated, further evaluations with CXR and echocardiogram are advised; annual rechecks are suggested if normal. These strategies facilitate early detection in T2DM patients, allowing prompt interventions to curtail heart failure progression.[8]
c. Addressing HF in Chronic Kidney Disease: Unique Window of Opportunity
In dialysis patients, heart failure is the second most prevalent cardiovascular disease, with incidences of 47.3% in peritoneal dialysis and 42.9% in hemodialysis, notably diminishing survival rates in these patients. China drafted their first guidelines for managing chronic heart failure in dialysis patients to address this, aiming to standardise treatment and enhance patient outcomes.[9]
They also focussed on cardiac biomarkers, such as NT-proBNP and high-sensitivity troponin, in identifying and prognosing heart failure within the CKD population. In dialysis patients, while elevated BNP levels indicate heart failure severity, adjusting the diagnostic threshold based on renal function is crucial. Research shows NT-proBNP indicates more heart failure than BNP, making it a preferable marker due to its longer half-life and higher plasma concentration. Though some studies suggest an NT-proBNP cutoff of 11215.2 ng/L for diagnosing heart failure in ESRD patients, its accuracy requires further validation in prospective studies and clinical settings.
Troponin T (TnT) offers better prognostic value than Troponin I (TnI) due to its higher sensitivity. In patients with renal insufficiency, hs-TnT levels rise slightly, necessitating adjusted prognosis cutoffs. Research indicates that a 40 ng/L threshold of hs-TnT is optimal for predicting mortality in CKD Stage 4 to 5 patients.[10]
Revolutionising Acute Coronary Syndrome Management through Troponin Rapid Algorithm
Prompt and precise diagnosis of suspected Acute Myocardial Infarction (AMI) is crucial for best patient outcomes and efficient emergency department (ED) management.
The innovative application of high-sensitivity troponin assays has transformed AMI diagnosis and risk assessment. By leveraging rapid troponin algorithms for quick decision-making, EDs can enhance patient care, ensuring swift interventions and better patient outcomes.
Backed by robust real-world evidence, the 2020 European Society of Cardiology (ESC) guidelines advocate for the 0h/1h hs-cTn algorithm over the older 0/3hr approach, emphasising its importance in rapid triage and efficient management of AMI patients.[10]
The DROP ASIAN ACS trial in Japan examines the benefits of using the 0-1-hr algorithm with hs-cTnT compared to conventional care in triaging patients with chest pain presenting to the EDs. This study aims to prove that the rapid algorithm can decongest EDs and reduce unnecessary admissions, bolstering clinician confidence in hs-cTn assays.
The transition to the new hs-cTn assay approach in the Department of Emergency and Intensive Care (DEIC) was facilitated by a customised Lab IT solution, a collaboration between Hanoi Medical University Hospital (HMUH), Vietnam and IVD Lab IT consultants. By prioritising blood samples for hs-cTn tests, results are available in under 30 minutes. This shift from manual to integrated systems enhances department coordination, ensuring efficient patient management and improved outcomes, as interpreted in the DROP-Asian ACS Study. Efforts are underway to refine ED triage for suspected ACS patients using advanced tools like AI-driven decision support.
Mitigating Perioperative Myocardial Injury
Perioperative myocardial infarction or injury (PMI) significantly impacts patients’ prognosis, with a 10% absolute increase in one-year mortality risk. The BASEL-PMI study revealed that, of those facing intermediate to high-risk surgeries, one in six patients would experience PMI. Alarmingly, only 20% displayed ischemic event symptoms, with a mere 6% reporting typical chest pain. Without proactive PMI screening, these cases could go unnoticed, leading to subsequent cardiovascular events, some fatal.[11]
The Revised Cardiac Risk Index has been the standard for over 15 years, and the most recent guideline reference was the 2014 ACC/AHA. However, the 2022 ESC guidelines offer a more precise and objective approach. Measuring hs-cTn before, as well as 24h and 48h, post-intermediate-to-high-risk NCS is strongly recommended to facilitate early detection of myocardial injury in non-cardiac surgical patients, enabling healthcare providers to take proactive measures.
The Bigger Picture: Collaborative Action
A holistic approach to CVD management necessitates seamless collaboration. Policymakers, care providers, healthcare organisations, pharmaceutical entities, governments, and patients must unite to ensure early detection, tailored treatment, and supportive post-care. This ensures that care delivery is continuous, comprehensive, and centred around the individual.
One such effort – The APAC CVD Alliance – champions heart health in Asia through collaborative endeavours that prioritise the well-being of patients at every stage.[12]
Conclusion
The utility of diagnostic parameters, such as NT-proBNP and cardiac high-sensitivity troponins, cannot be overstated. These biomarkers are essential for accurate diagnosis and have significant implications for improving CVD management. However, bridging the gap between current standards of care and the desired excellence in the APAC region demands a concerted effort from multiple stakeholders. Fortunately, with the tools and knowledge at our disposal, we can drive significant improvements in cardiovascular health across APAC. As we chart the path forward, we remain optimistic and committed to fostering a future with enhanced heart health for all in the region.