What is the current state of heart failure management in India? And what in your opinion are some of the biggest unmet needs in this field?
The current prevalence of HF in India is estimated to be around 10 million. Coronary heart disease, hypertension, diabetes and rheumatic heart disease being the most common causes. In the INTER-CHF a global study the one-year mortality in HF patients was highest in Africa (34%) followed by India (23%). Indian patients with HF are younger, present late with severe symptoms, often have little education, negligible health insurance and still being treated frequently with digoxin alone. In the Trivandrum Heart failure registry of 1250 patients with HF only 25% were receiving guideline directed treatment (GDMT). The 5-year mortality of the patients included in this registry was 59%.
Some of the biggest unmet needs include:
- Lack of Public Awareness
- Delay in the diagnosis
- Lack of serious efforts to put patients on GDMT at the earliest
- Inadequate facilities for hospitalization
- Negligible remote monitoring facilities after starting treatment
- Lack of a multidisciplinary team to guide and evaluate
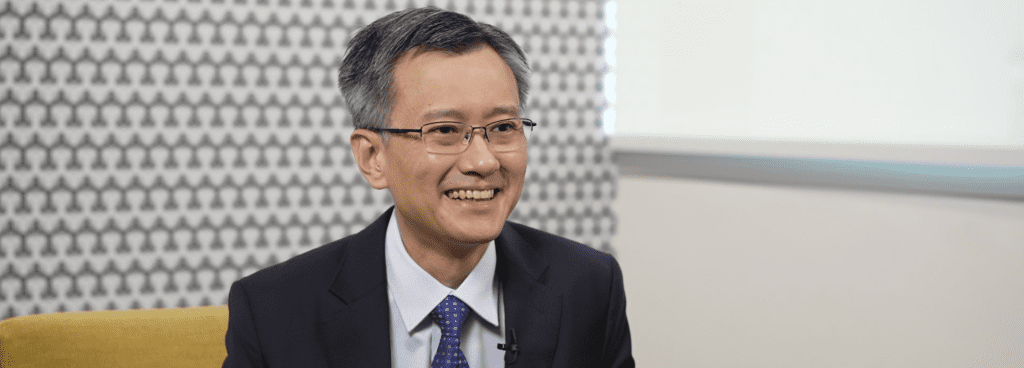
How is Dr Upendra Kaul leading the way in addressing HF management gaps in India?
Patients with acute decompensated heart failure are always admitted in our Batra Heart Center for acute assessment and prompt management using the GDMT started at the earliest and an attempt is made to start all of them within a few weeks of discharge if not earlier. Much depends upon their hemodynamic status, renal function and other comorbidities which they often have. Elderly population poses additional problems like frailty, polypharmacy and cognitive issues. Thereby an individualized treatment algorithm is to be initiated.
Our experience with biomarkers and their use not only in hospital practice but also in camps and the centers in remote areas set up by our NGO, Gauri Kaul Foundation has been very gratifying. These point of-care tests readily diagnose and differentiate HF from many other conditions mimicking it. The test also gives a reliable idea about the severity of the illness and after starting the GDMT helps in follow- up and can be used for remote monitoring. We use this test through Telemedicine centers put in remote areas and guiding the treatment digitally.
Besides this a periodic monitoring of the renal function especially the creatinine clearance and electrolytes is needed. Heart failure is frequently associated with renal dysfunction and drugs used to treat like ACE inhibitors and aldosterone antagonists can lead to hyperkalemia.
How do you envision the results of the STRONG-HF study would potentially affect the way heart failure is managed in India, and what do you think are the potential barriers to widespread adoption of these recommendations?
STRONG- HF is a prospective study thus clearly shows the importance of early aggressive therapy for ADHF patients and should have a substantial impact on clinical practice and, if adopted and implemented worldwide, on outcomes for patients with heart failure. The messages conveyed by this trial and the previous suggestions made by experts of initiating all the drugs early and in any case by 4 weeks, need to be brought to light to the Indian doctors managing the patients with HF. The regimen suggested in STRONG -HF trial should be propagated through in several geographies of the country. The concerns of the clinicians to start drugs and build up their dosages rapidly in order to get the best benefit needs to be allayed. They need to be reassured that serious adverse effects are unlikely although transient hypotension or low heart rate may be seen which can be overcome easily by proactive initial monitoring.
How would Dr Kaul advise the integration of the follow up recommendations as per STRONG-HF study into clinical practice in the Indian healthcare setup?
The STRONG -HF trial results need to be conveyed and highlighted to the practicing physicians and cardiologists by well-known and reputed speakers. This can be done initially by selecting key opinion leaders and making appropriate scientific programs involving the local physicians and cardiologists. Forums like Cardiological Society of India and other national meetings like the Association of Physicians of India need to be involved.
Involving the internists in these programs as panellists is very important because they are persons who follow up these patients and, in many hospitals, also manage patients with ADHF. They need to be kept abreast of the fact that management has much more to offer than just the use of diuretics and digitalis and they can start these agents if there is a delay in referring them to hospitals and cardiologists.
Social media for mass awareness like Facebook, LinkedIn and Twitter should be brought in and highlight how sick heart failure patients need an early optimal treatment with improved survival and reduced hospitalization.
How would you advise your peers in Asia Pacific on optimising GDMT for their HF patients for better outcomes?
The mortality of heart failure is high throughout. The results of STRONG HF study should be universally applicable. Many of the health care systems in APAC have many things in common andcertainly need adoption of the aggressive and rapid institution of drugs along with general measures of Follow up.
With the availability of drugs to manage ADHF, chronic heart failure and worsening HF the future of these sick patients is poised to improve, better QOL, less hospitalizations and improved survival.
Adoption of drugs such as ACEI/ARBs/ARNI , beta blockers, SGLT2i , Aldosterone antagonists and now an oral soluble guanylate cyclase stimulator (Verciguat) in clinical practice is the key along with timely monitoring with the appropriate use of biomarkers. National registries would be an additional help to generate more scientific data for patients with ADHF in the real world.