Cardiovascular diseases are the leading cause of death globally, accounting for an estimated one-third of deaths worldwide. Heart failure (HF) represents the end phenotype of various cardiovascular diseases and it is also the most common cause of hospitalization in people aged >65 years. Despite advances in care, short- and long-term mortality rates remain significant in patients with HF. Studies have shown that HF had a similar or worse 5-year survival rate compared to many of the cancers1.
Between 1990 and 2019, the number of HF cases in China has significantly increased, with the total prevalent cases rising from 7.03 million in 1990 to 18.51 million in 20192. Over the years, HF has placed a remarkable economic burden on the healthcare systems in China, thus it is crucial to have a standardized protocol for clinical management in HF throughout the disease course, especially during the acute phase that is associated with high mortality.
Prof Alexandre Mebazaa recently shared the results of the STRONG-HF study during a speaker tour in China, to help Chinese physicians discern the study and the implementation of intensification of treatment strategies for patients with acute HF post-discharge.
The Significance of the STRONG-HF Study
The STRONG-HF was a multinational, multicenter, open-label, randomized, parallel-group study showing that most patients admitted for acute HF and not treated with optimal doses of oral HF therapies can be rapidly and safely up-titrated to recommended doses of drugs within a few weeks after discharge, followed by frequent visits comprising clinical and laboratory assessments, including NT-proBNP3.
Based upon the trial results, the 2023 Focused Update of the ESC Guidelines for the diagnosis and treatment of acute and chronic HF recommends high-intensity care for initiation and rapid up-titration of oral HF therapies and close follow-up in the first 6 weeks after discharge from an acute HF hospitalization, in order to reduce HF readmission or all-cause death, with a class 1 recommendation and level B evidence. During the follow-up visits, particular attention should be paid to symptoms and signs of congestion, blood pressure, heart rate, NT-proBNP values, potassium concentrations, and eGFR4.
NT-proBNP as a Vital Marker in the Management of HF
The recent universal definition of HF position paper specifies an ambulatory NT-proBNP above 125 pg/mL as a corroborating factor when accompanied by symptoms or signs of the disease5. Prof Mebazaa shared his perspective on the role of NT-proBNP, that it is a reliable biomarker to be used in tracking the treatment of HF as it can provide real-time feedback regarding the effectiveness of therapy. It is safe and effective to use NT-proBNP testing in guiding the management across the spectrum of HF stages.
The expert panels from China shared that NT-proBNP is now a versatile biomarker being used locally in different scenarios. For diagnostics, the measurement of NT-proBNP has been increasingly used for the management of patients presenting to an emergency room with dyspnea or other symptoms suggestive of HF to distinguish acute HF from other conditions. Besides, NT-proBNP is an evaluation tool for assessing the effectiveness of HF therapy, for example, a patient experiencing symptom relief under treatment but found with rising NT-proBNP might suggest that there is another underlying cause for HF that needs to be resolved. Furthermore, the role of NT-proBNP in guiding dosage adjustment of medications during the acute phase of HF has been validated in the STRONG-HF study.
Current Situation and Dilemmas on Implementing Guideline-Directed Medical Therapy (GDMT) for HF in China
The establishment of the HF center in China started in 2017. At present, there are more than 700 units accredited by China Heart Failure Center to provide holistic care to patients with HF. In these hospitals, patient data and management for HF are required to be recorded in a registration system, in order to have a better understanding of the demographics and clinical characteristics of patients hospitalized with HF and to evaluate the management in different regions and hospitals. The registry provides insights into the gaps and opportunities to improve clinical practice in HF.
Despite the real-world data analysis showing the diagnosis and treatment level of HF in China has significantly improved overall in the past years, there remain large gaps in the standardization of care for patients hospitalized for HF6. In addition, although accelerating the safe implementation of GDMT has proven to reduce the morbidity and mortality associated with HF in high-level randomized evidence and international guidelines, it remains an ongoing challenge for patients, clinicians, and healthcare systems in China7.
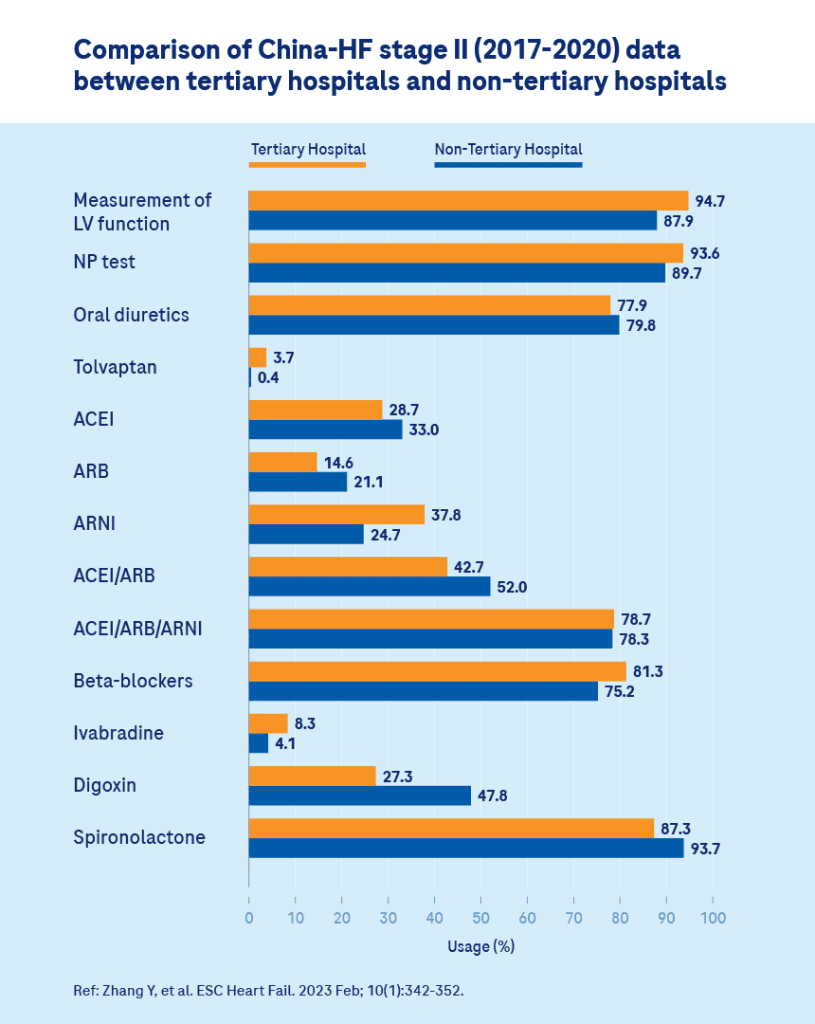
Ref: Zhang Y, et al. ESC Heart Fail. 2023 Feb;10(1):342–352.
China-HF registry (2017–2020) included 29,728 patients (85.1%) from 87 tertiary hospitals and 5210 patients (14.9%) from 26 non-tertiary hospitals. The figure shows utilization rates of LV function measurement, natriuretic peptide test, oral beta-blockers, tolvaptan, and ivabradine at discharge for appropriate patients were higher in tertiary hospitals than those in non-tertiary hospitals, whereas oral traditional diuretics, spironolactone, and digoxin were lower in tertiary hospitals (P < 0.05).
There are several patient-related factors causing the delay of optimal target dosing in GDMT implementation, including drug intolerance or side effects, comorbidities, advanced age, frailty, etc. Furthermore, the underutilization of GDMT may partly stem from the imbalances of health resources. During the talk, Prof Mebazaa emphasized that patients with acute HF would encounter a high mortality risk if not given the optimal dosage of treatment, and it is highly recommended that targeted interventions in compliance with guidelines should be developed to improve HF management in China.
Overcoming Apprehensions for HF treatment in China
In the panel discussion regarding the optimization of HF management in China, the experts have proposed a few key strategies to tackle the obstacles. First, more accredited HF centers should be developed across the country to provide standardized protocols for managing HF, and HF professionals or multidisciplinary teams are required to be well-equipped with updated knowledge, to ensure each center works toward the adoption of and compliance with the latest guidelines.
In addition, close collaboration among tertiary centers and local clinics or primary care centers should be implemented, in order to provide comprehensive care for patients with HF living in rural areas. This allows the patients to visit on time following discharge from acute HF admission, and receive an adequate evaluation for medication dosage adjustment. It is gratifying to note that NT-proBNP testing is currently available at clinics in most of the rural areas of China, enabling physicians to utilize it as a powerful tool in considering the up-titration of recommended doses of drugs in patients with acute HF post-discharge.
From a clinical aspect, NT-proBNP testing is considered well-established in most of the health centers in China, and physicians are advised to dive deeper to investigate how to use the testing at the early stage of the disease, or the frequency of using it when facing changes in patients’ condition throughout the whole treatment process. From the perspective of scientific research, it is paramount to have more in-depth research for further validation of the role of NT-proBNP in guiding HF therapy or suggestion of targeted populations that are more likely to benefit from the testing. From a production aspect, it is essential to ensure the standardization of NT-proBNP assays and the accessibility of this laboratory testing across healthcare facilities in China for rapid diagnosis, management, and surveillance of HF.
Currently, there is a disparity in managing acute HF in China, as many physicians experience clinical inertia in performing rapid dose escalation of guideline-recommended therapies. The implication of the STRONG-HF study is that the protocol for the effective management of acute HF was created in an objective manner and it proves that rapid up-titration of recommended doses of drugs with close follow-up and monitoring could lead to better outcomes and prognosis in patients. However, physicians are advised to cautiously select patients who are eligible to receive this treatment strategy and observe the treatment tolerability and clinical outcomes in the Chinese population.
The Road Ahead
With the positive results, physicians are encouraged to start adopting the strategy of acute HF management from the STRONG-HF study in a stepwise approach. It is necessary to provide training courses for medical professionals so that they can understand the value of optimizing GDMT in the management of HF. As physicians start implementing the strategy in a small cohort of patients, it is believed that they will become more confident and experienced in assembling drug combinations for effective HF therapy. Besides, patient education needs to be prioritized to help individuals understand the proper ways for self-managed care and avoid non-essential readmissions. In addition, local studies with larger populations could be performed to validate the safety and effectiveness of rapid up-titration of GDMT combining clinical and laboratory assessment in Chinese patients with acute HF.
Given the wide availability of the medication and physicians are well-equipped with profound medical knowledge in treating acute HF, it is believed that the implementation of the STRONG-HF study protocol could easily and rapidly achieve better patient outcomes in China.